National Colorectal Cancer Month
Most Canadians don’t like to talk about colorectal cancer but the month of March is a great time to change that. March is national Colorectal Cancer Awareness month, and this is a great time for survivors, patients, caregivers, and everyone who has been affected by this disease to tell their story and to talk about a disease that is preventable, treatable and beatable. These conversations can save lives!
Understanding Colorectal Cancer
The Colon and Rectum
The colon and rectum perform vital functions in the last phases of digestion. Digestion first begins in the mouth where food is chewed into smaller pieces and swallowed. The food travels down the esophagus to the stomach where it is further broken down by gastric juices and sent to the small intestine. The small intestine continues to break down the contents in addition to absorbing most of the nutrients, including carbohydrates, proteins and vitamins. Once the contents have passed through the small intestine, the material has become mostly liquid and is moved into the colon, which measures about 5 ½ feet long. The main function of the colon is to absorb water and dehydrate the leftover material, forming semi-solid matter, or stool. The colon moves the stool into the approximately 6-inch long rectum, which acts as a holding chamber, until it is ready to be expelled through the anus.
Colorectal Cancer
Because colon and rectal cancers arise from the same type of cell and have many similarities, they are often referred to collectively as “colorectal cancer”. The cells lining the colon or rectum can sometimes become abnormal and divide rapidly. These cells can form benign (non-cancerous) tumours or growths called polyps. Although not all polyps will develop into colorectal cancer, colorectal cancer almost always develops from a polyp. Over a period of many years, a polyp’s cells may undergo a series of DNA changes that cause them to become malignant (cancerous). At first, these cancer cells are contained on the surface of a polyp, but can grow into the wall of the colon or rectum where they can gain access to blood and lymph vessels. Once this happens, the cancer can spread to lymph nodes and other organs, such as the liver or lungs-this process is called metastasis, and tumours found in distant organs and called metastases.
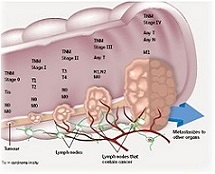
Staging Colorectal Cancer
Staging describes the extent of the cancer based on how many layers of the bowel wall are affected, whether lymph nodes are involved, and if there is spread to other organs. For colorectal cancer, staging often can’t be completed until after surgery to remove the primary tumour along with surrounding tissue (containing lymph nodes), and possibly lesions found on other organs. A pathologist studies the surgical specimen(s) to determine the stage. The most frequently used, and most precise staging system for colorectal cancer, is the TNM system. TNM stands for Tumour Nodes Metastases and the system describes the extent of each using numbers; the higher the number, the more of the element that is affected:

After each element has been determined, they are combined to form and overall stage of the cancer in roman numerals, the higher the number, the more advanced the cancer. This is generally how the cancer is referred to between doctor and patient:
· 0 – The cancer is confined to the innermost layer of the colon or rectum. It has not yet invaded the bowel wall.
· I – The cancer has penetrated several layers of the colon or rectum wall.
· II – The cancer has penetrated the entire wall of the colon or rectum and may extend into nearby tissue(s).
· III – The cancer has spread to the lymph nodes.
· IV – The cancer has spread to distant organs, usually the liver or lungs.
What are the Risk Factors for Colorectal Cancer?
A risk factor is something that increases a person’s chances of developing a disease such as colorectal cancer. Not all cancers have the same risk factors associated with them. For example, exposing the skin to the sun is a risk factor for skin cancer and smoking is a risk factor for cancer of the lungs.
The exact causes of colorectal cancer are not known. However, studies show that the following risk factors increase a person’s chances of developing colorectal cancer and they have been divided into two main categories: those risk factors that you cannot change and those that are lifestyle-related and therefore subject to change/alteration. A third category at the end lists those risk factors that have yet to be substantiated by medical research and are somewhat controversial, but have been included for the purpose of promoting awareness.
Risk Factors You Cannot Change
· Age – The risk of developing colorectal cancer increases as one ages. The disease is more common in people over the age of 50, and the chance of developing colorectal cancer increases with each decade. However, colorectal cancer has also been known to develop in younger people as well (Patel, 2009: Gairdiello, 2008)
· Personal History of Colorectal Polyps/Cancer – Polyps are non-cancerous growths on the inner wall of the colon or rectum. While they are fairly common in people over 50, one type of polyp, referred to as an adenoma, increases the risk of developing colorectal cancer. Adenomas are non-cancerous polyps that are considered precursors, or the first step toward colon and rectal cancer. Also, a person who already has had colorectal cancer may develop the disease a second time in other areas of the colon or rectum. The chances of this happening are greater if you had your first colorectal cancer when you were younger than age 50. (Eide et al, 2006)
· Personal History of Inflammatory Bowel Disease – Long standing inflammatory diseases of the colon, such as Ulcerative Colitis and Crohn’s Disease, can increase your risk of colon cancer. Both ulcerative colitis and Crohn’s are conditions in which the lining of the colon become inflamed over a long period of time. Your risk of developing colorectal cancer therefore increases, as does your need to be screened for the disease on a more frequent basis. (S. Itzkowitz et al, 2004)
· Family History of Colorectal Cancer - First degree relatives (parents, siblings, children) of a person who has had colorectal cancer are somewhat more likely to develop this type of cancer themselves, especially if the relative had the cancer at a young age. If many family members have had colorectal cancer, the chances increase even more. In some cases, the connection may not be hereditary or genetic. Instead, cancers within the same family may result from shared exposure to an environmental carcinogen (cancer-causing agent) or from diet or lifestyle factors. (J. Olsen et al. 2004)
· Inherited Syndromes - Genetic syndromes passed through generations of one’s family can increase one’s risk of developing colon cancer. These syndromes cause only approximately 5% of all colon cancers. The two most commonly inherited syndromes linked with colorectal cancers are: Familial adenomatous polyposis (FAP) and hereditary non-polyposis colorectal cancer (HNPCC).
Familial Adenomatous Polyposis (FAP): is a rare disorder that causes you to develop hundreds to thousands of polyps in the lining of your colon and rectum, usually in your teens or by early adulthood. People with untreated FAP have a greater than 90% chance of developing colon cancer in one of those polyps by age 45 and accounts for 1% of all colorectal cancers. The development of colorectal cancer can be avoided by employing preventive surgery (removal of the colon). (A. Kinney et al., 2007)
Hereditary Non-Polyposis Colorectal Cancer (HNPCC): also called Lynch Syndrome is more common than FAP. People with HNPCC have an increased risk of colon cancer and tend to develop colon cancer at an early age. It accounts for about 3-4% of all colorectal cancers but there are not as many polyps developed in the colon as there are in FAP. The lifetime risk of colorectal cancer in people with this condition may be as high as 70-80%. (M. Scheurhen et al., 2001)
There is another rare inherited condition called Peutz-Jeghers Syndrome. People with this condition tend to have freckles around the mouth (and sometimes on the hands and feet) and large polyps in their digestive tracts. They are at greatly increased risk for colorectal cancer; as well as several other cancers, which usually appear at a younger than normal age. (L. Boardman et al., 1998)
· Racial & Ethnic Background - African Americans have the highest colorectal cancer incidence and mortality rates of all racial groups, especially in the U.S. The reason for this is not yet understood. (E. Mitchell, et al., 2009)
Jews of Eastern European descent (Ashkenazi Jews) have one of the highest colorectal cancer risks of any ethnic group in the world. Several gene mutations leading to an increased risk of colorectal cancer have been found in this group. (I. Shapira et al., 2002; DS. Weinberg et al., 2006)
· Personal History of Other Cancers - Research shows that women who have a history of ovarian, uterine, endometrial or breast cancer have a somewhat increased risk of developing colorectal cancer. Therefore, it is imperative that special screening guidelines be adhered to for this subgroup of patients. (M. Manuel et al., 2007)
Lifestyle-Related Risk Factors That Can Be Altered
· Diet - Colorectal cancer appears to be associated with diets that are high in fat and calories, red and processed meats and low in fiber, vegetables and fruits. Researchers have also suggested that methods of cooking meats at very high temperatures (frying, broiling or grilling) create chemicals that might increase cancer risk. For a more thorough discussion of preventing colorectal cancer through a healthy lifestyle, please visit the Nutrition & Exercise Section of this website. (Kouskik, 2008; Langman 2002; Vinikoor 2008
· Sedentary Lifestyle/Physical Inactivity - If you are inactive, you are more likely to develop colon cancer. This may be because when you are inactive, waste (fecal material) has a tendency to stay in your colon longer. Obtaining regular physical activity may reduce your risk by stimulating the movement of your colon and the passage of waste through the colon. (Salz et al., 2006; Giovannucci et al., 2006)
· Type II Diabetes - People with type 2 (usually non insulin dependent) diabetes may have an increased risk of developing colorectal cancer. Both type 2 diabetes and colorectal cancer share some of the same risk factors (such as excess weight). But even after taking these into account, people with type 2 diabetes still have an increased risk. (Liu et al., 2008)
· Obesity - People who are obese have an increased risk of colon cancer and an increased risk of dying of colon cancer when compared with people considered normal weight. (Pasche et al., 2008)
· Smoking - Long-term smokers are more likely than non-smokers to develop and die from colorectal cancer. While smoking is a well-known cause of lung cancer, some of the cancer-causing substances are swallowed and can cause digestive system cancers, such as colorectal cancer. (Botteri et al., 2008)
· Severe Alcoholic Consumption - Colorectal cancer has been linked to the heavy use of alcohol. At least some of this may be due to the fact that heavy alcohol users tend to have low levels of folic acid in the body. Still, alcohol use should be limited to no more than 2 drinks per day for men and 1 drink per day for women. (Bongaerts et al., 2008)
Factors with Uncertain, Controversial, or Unproven Effects on Colorectal Cancer
· Growth Hormone Disorder - Acromegaly, an uncommon disorder that causes an excess of growth hormone in your body, may increase your risk of colon polyps and colon cancer.
· Night Shift Work - Results of one study suggested working a night shift at least 3 nights a month for at least 15 years may increase the risk of colorectal cancer in women. The study authors suggested this might be due to changes in levels of melatonin (a hormone that responds to changes in light) in the body. More research is needed to confirm or refute this finding.
· Previous Radiation Therapy for Certain Cancers - Radiation therapy directed at the abdomen to treat previous cancers may increase the risk of colon cancer. Some studies, for example, have found that men who survive testicular cancer seem to have a higher rate of colorectal cancer and some other cancers. This might be due to the treatments they have received. Some early studies suggested that men who received radiation therapy to treat prostate cancer might have a higher risk of rectal cancer, as the rectum receives some radiation during treatment.
Research has led to real progress against this increasingly treatable disease, with a lower chance of death and an improved quality of life for the people who have it. Whatever your risk factors may be, leading a generally healthy lifestyle, as advocated in the Healthy Lifestyle Section, and seeking regular screening will be among the best preventive actions you can take to reduce your chances of being affected by colorectal cancer.
Click here to learn more about Colorectal Cancer
Source: Colorectal Cancer Association of Canada